Since the news about the air traffic controllers a few weeks ago, it seems like the topic of sleep is being discussed everywhere. When I initially evaluate my patients I ask about their sleep habits and make recommendations on which positions might be the best and those to avoid. The position in which one chooses to sleep can sometimes be the cause of the problem for which he or she is seeking treatment. Though I believe sleep posture and appropriate positioning is important for treating certain conditions, I was curious to know if quality and quantity of sleep impacts a person’s outcome in physical therapy. I value sleep personally and believe it does have an impact on how well someone can recover. I looked at research to learn more about sleep and to see if this topic has been investigated as it relates to physical therapy. I learned a few interesting things.
The exact purpose of sleep remains elusive. Our sleep cycle consists of periods of REM and non-REM sleep1 During sleep we alternate between REM (rapid eye movement) and non-REM (non-rapid eye movement) sleep with increased duration of REM sleep towards the end of the night. A component of non-REM sleep is short wave sleep, which some researchers hypothesize has physiological restorative benefits. This type of sleep diminishes as one ages.2 The amount of sleep one needs can vary with some people, “short sleepers,” only needing 4-6 hours of sleep per night versus others needing 7-9 hours. Current research indicates that it is rare to be a true “short sleeper,” but many more people think they are one and are really depriving themselves of sleep. One possible indication that you are not a “short sleeper”: if you prefers to sleep in over the weekend versus only sleeping 4-6 hours per night as you might during the work week, then you are probably depriving yourself sleep during the work week.3
Sleep can have a positive effect on motor learning in young, healthy people, with a 60-90 minute nap improving performance. Research has also indicated this same beneficial effect of sleep is seen in people recovering from stroke.4 Patients recovering from stroke often have to relearn many movements including things like walking, grasping objects with their hands, and getting up and down curbs. Though research suggests the positive effects of sleep on learning motor skills and movements, which could benefit physical therapy, I also wondered what the negative effects would be of not getting adequate sleep.
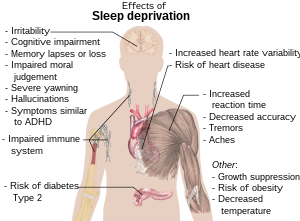
Research suggests the negative effects of sleep deprivation include:
- increased risk of weight gain5
- alteration of immune system6
- increased perception of anxiety and depression7
- increased inflammatory cells in the body8
- impaired memory and concentration9
- increase in muscle tone10
- muscle tremor11
- difficulty maintaining balance12
- increased sensitivity to pain13
58% of people with low back pain were found to have sleep disturbance.14 Sleep disturbance is also common in cases of rheumatoid arthritis.15 Although research shows that people with these conditions have disturbed sleep, I could not find studies that investigated the effect of sleep on the condition. Based on the research of the effect of sleep deprivation, I would think that not having enough sleep would impact physical therapy outcomes, though I could not find much research on the effects of sleep deprivation on these conditions.
In summary, sleep does appear sleep has some positive benefits in learning motor skills in young, healthy people and in people recovering from stroke. I was not able to find research that touts the benefits of sleep on outcomes in physical therapy. From the few articles I did read, it seems that there are more negative consequences of sleep deprivation than positive effects. I couldn’t find too many studies that investigated the effect of sleep deprivation on physical therapy outcomes. However, many of the negative consequences mentioned in the research articles including weight gain, inflammation, impaired memory, and altered muscle tone suggest that depriving oneself of sleep could have a negative impact on the outcome of physical therapy. As our lifestyles demand so much of our time, we can’t forget to take care of ourselves including saving adequate time for catching needed, restorative sleep.
Related articles
- Tired Neurons Caught Nodding Off in Sleep-Deprived Rats (nlm.nih.gov)
- Memory lapses linked to napping brain cells (cbsnews.com)
- Short sleep is linked with premature death (bhls.wordpress.com)
- Siengsukon & Boyd. (2009). Does Sleep Promote Motor Learning? Implications for Physical Rehabilitation. Phys Ther. 89: 370-383. [↩]
- Ranjbaran, Keefer, Stepanski, Farhadi, & Keshavarzian. (2007). The relevance of sleep abnormalities to chronic inflammatory conditions. Inflamm. Res. 56:51-57. [↩]
- Beck, Melinda. “The Sleepless Elite.” Wall Street Journal, Apr 5, 2011. [↩]
- Siengsukon & Boyd. (2009). Does Sleep Promote Motor Learning? Implications for Physical Rehabilitation. Phys Ther. 89: 370-383. [↩]
- Orzel-Gryglewska. (2010). Consequences of sleep deprivation. International Journal of Occupational Medicine and Environmental Health; 23 (1): 95-114. [↩]
- Ranjbaran, Keefer, Stepanski, Farhadi, & Keshavarzian. (2007). The relevance of sleep abnormalities to chronic inflammatory conditions. Inflamm. Res. 56:51-57. [↩]
- Orzel-Gryglewska. (2010). Consequences of sleep deprivation. International Journal of Occupational Medicine and Environmental Health; 23 (1): 95-114. [↩]
- Ranjbaran, Keefer, Stepanski, Farhadi, & Keshavarzian. (2007). The relevance of sleep abnormalities to chronic inflammatory conditions. Inflamm. Res. 56:51-57. [↩]
- Orzel-Gryglewska. (2010). Consequences of sleep deprivation. International Journal of Occupational Medicine and Environmental Health; 23 (1): 95-114. [↩]
- Orzel-Gryglewska. (2010). Consequences of sleep deprivation. International Journal of Occupational Medicine and Environmental Health; 23 (1): 95-114. [↩]
- Orzel-Gryglewska. (2010). Consequences of sleep deprivation. International Journal of Occupational Medicine and Environmental Health; 23 (1): 95-114. [↩]
- Orzel-Gryglewska. (2010). Consequences of sleep deprivation. International Journal of Occupational Medicine and Environmental Health; 23 (1): 95-114. [↩]
- Orzel-Gryglewska. (2010). Consequences of sleep deprivation. International Journal of Occupational Medicine and Environmental Health; 23 (1): 95-114. [↩]
- Alsaadi, S., Mcauley, J., Hush, J., & Maher, C.. (2011). Prevalence of sleep disturbance in patients with low back pain. European Spine Journal, 20(5), 737-743. [↩]
- Ranjbaran, Keefer, Stepanski, Farhadi, & Keshavarzian. (2007). The relevance of sleep abnormalities to chronic inflammatory conditions. Inflamm. Res. 56:51-57. [↩]











April 29, 2011
General Information, Prevention